 The stethoscope, invented in 1816, is getting an update with the Food and Drug Administration’s approval of the Eko Core — a digital device that attaches to a conventional stethoscope and allows it to record, amplify, and wirelessly send audio and sound wave images to a smart phone. The patient’s heart sounds can be visualized, recorded, saved, and shared using the Eko iPhone and iPad App. It also has the ability to store the heart sounds in a patient’s electronic medical record so doctors can compare sounds from a recent visit with ones from a year or two earlier. With FDA approval, Eko Health, a startup led by three recent University of California graduates, can now market its Littmann® CORE digital stethoscope. Cardiologists at the Mayo Clinic, Stanford, and the University of California, San Francisco who have sampled the new technology have been impressed. “This is probably one of the most important innovations in the plain old stethoscope in recent years” according to Dr. Charanjit Rihal, chairman of the department of cardiovascular disease at the Mayo Clinic.
The stethoscope, invented in 1816, is getting an update with the Food and Drug Administration’s approval of the Eko Core — a digital device that attaches to a conventional stethoscope and allows it to record, amplify, and wirelessly send audio and sound wave images to a smart phone. The patient’s heart sounds can be visualized, recorded, saved, and shared using the Eko iPhone and iPad App. It also has the ability to store the heart sounds in a patient’s electronic medical record so doctors can compare sounds from a recent visit with ones from a year or two earlier. With FDA approval, Eko Health, a startup led by three recent University of California graduates, can now market its Littmann® CORE digital stethoscope. Cardiologists at the Mayo Clinic, Stanford, and the University of California, San Francisco who have sampled the new technology have been impressed. “This is probably one of the most important innovations in the plain old stethoscope in recent years” according to Dr. Charanjit Rihal, chairman of the department of cardiovascular disease at the Mayo Clinic.
Source: “With New Stethoscope, Take a Deep Breath, Then Consult Your Phone” by Steve Lohr, The New York Times, September 3, 2015.
This article is an update of a previous post.

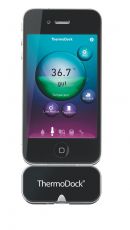 With the Medisana ThermoDock® a healthcare provider is one step closer to having a medical toolkit like Dr. McCoy on Star Trek. The ThermoDock provides reliable and accurate measurement of body temperature with non-contact infrared technology and plugs into an iPhone®, iPod touch® or iPad® — at a safe distance from flu germs, grumpy children, and steaming coffee mugs. Although a certified medical device and typically pointed at a forehead, this gadget can also be used to check the ambient temperature of a room or the great outdoors and has a memory for storing multiple user profiles. The ThermoDock works with the free VitaDock® app to track data and the hardware component costs less than $100.
With the Medisana ThermoDock® a healthcare provider is one step closer to having a medical toolkit like Dr. McCoy on Star Trek. The ThermoDock provides reliable and accurate measurement of body temperature with non-contact infrared technology and plugs into an iPhone®, iPod touch® or iPad® — at a safe distance from flu germs, grumpy children, and steaming coffee mugs. Although a certified medical device and typically pointed at a forehead, this gadget can also be used to check the ambient temperature of a room or the great outdoors and has a memory for storing multiple user profiles. The ThermoDock works with the free VitaDock® app to track data and the hardware component costs less than $100. At the Johns Hopkins Hospital (JHH), in the center of their campus in Baltimore, Maryland, is a room with walls made of 22 high-resolution screens. Numbers, charts and live video flash across them as about 24 staff members from different departments scan the screens and make quick decisions to prevent or resolve bottlenecks, reduce patient wait time, coordinate services and reduce risk. During a typical afternoon, the system receives about 500 messages per minute from 14 different Johns Hopkins IT systems generating real-time data to trigger action throughout the hospital.
At the Johns Hopkins Hospital (JHH), in the center of their campus in Baltimore, Maryland, is a room with walls made of 22 high-resolution screens. Numbers, charts and live video flash across them as about 24 staff members from different departments scan the screens and make quick decisions to prevent or resolve bottlenecks, reduce patient wait time, coordinate services and reduce risk. During a typical afternoon, the system receives about 500 messages per minute from 14 different Johns Hopkins IT systems generating real-time data to trigger action throughout the hospital.